
The Global Health Committee (GHC) had its beginnings in 1994 as the Cambodian Health Committee (CHC), which began its work in the tuberculosis (TB) wards of three district hospitals in rural Svay Rieng province in eastern Cambodia, bordering Vietnam. With an expansion to Africa, the Global Health Committee name was established in 2008 to reflect its worldwide focus. In Cambodia, the name CHC continues to be used.
CHC has treated more than 32,000 people infected with TB in Cambodia, and today provides primary HIV care for more than 4,300 adults and 1,000 children in Svay Rieng, once devastated by the Vietnam War, and Kompot, another war-impacted province where the Khmer Rouge actively fought until 1997, and in Phnom Penh, the capital city. When CHC first arrived in Svay Rieng it had one of the highest rates of TB in the world.
GHC began its work in Ethiopia in 2008. As of April 2013, more than 700 patients have been started on therapy for drug-resistant TB in a pioneering program in cooperation with the country's Ministry of Health, which established drug-resistant TB care in the country, which is one of the poorest on earth and has the seventh highest burden of TB globally. This program follows the model of success CHC earlier established in Cambodia.
The organization's success lies in its community-based approach, pioneering this first-of-its-kind model of community-based care and treatment that has its roots in the refugee camps of the Thai-Cambodia border n the 1980s. CHC discovered that the strong community ties and tight-knit extended families that characterize the region is a treasured resource that can be leveraged to achieve strong results even in a war zone.
Building on the success of its TB program, CHC applied that same novel approach to treat AIDS while employing cutting edge tools and technologies of science to discover new and more effective therapies. Today, the organization persists in pioneering new ways to care for people with TB/AIDS in hard-to-access rural areas.
GHC's TB and AIDS treatment programs and advocacy work continue to promote innovative approaches to treating infectious diseases in partnership with families and communities. Our research has revealed answers to the many scientific questions about TB and HIV infection. In particular, the CAMELIA (Cambodian Early versus Late Introduction of Antiretrovirals) study, led by the CHC in partnership with French colleagues and support by the French ANRS and the NIH in the US, has provided an answer to the optimal timing of drugs for TB/HIV and is expected to save more than 150,000 lives this year alone.
Moving forward GHC/CHC will continue its relentless pursuit to attack TB, AIDS and the root causes of these diseases in adults and children in Asia and Africa, giving people the knowledge and access to medicines to allow them to lead healthy lives.
| 2012 | Cambodia The year 2012 is significant in Cambodia’s fight to eradicate TB. The World Health Organization in its 2012 Global Tuberculosis Report held up Cambodia as a global example in eradicating TB for its 45% drop in TB prevalence between 2002 and 2011, which is due in large part to the countrywide scale-up of the CHC’s Community Treatment Model that CHC developed and piloted. Although Cambodia has made significant progress, it remains among the 22 countries in the world with a high burden of tuberculosis. CHC has now treated more than 38,000 people for TB since its founding in 1994, and continues to deliver direct TB care to an area serving nearly two million people in three of Cambodia's poorest and most war-affected provinces, Svay Rieng, Kompot, and Kandal. CHC’s other programs in Cambodia continue to provide care for thousands of children and adults with HIV or TB and drug resistant TB. The Maddox Chivan Children’s Center (MCCC) continues to grow and thrive, providing its unique programs of multidisciplinary outpatient and social/educational care to nearly 1,100 Cambodian children infected or affected by HIV/AIDS, a quarter of whom are HIV+. The MCCC program is integrated with the CHC’s Khmer Soviet Friendship Hospital’s pediatric ward and Sullivan outpatient center, which provides primary care to more than 400 HIV+ children. And the Pulmonary Center of Excellence, also at the Khmer Soviet Friendship Hospital, admitted more than 700 patients in 2012, serving more than 3,300 patients since its opening in 2005. CHC is now responding to the cost of health care, the major cause of rural debt in Cambodia and other resource-poor countries, implementing an expansive community-based health insurance (CBHI) program in 2011. Underscoring the great need this program addresses, more than 6,460 families – 28,000 individuals – took advantage of the program during 2012, receiving a subsidy for their health care; thus protecting their families from the financial ruin that often accompanies the illness of a child or other family member. |
|
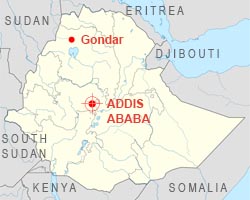
| 2012 | Ethiopia At the close of 2012, GHC reached a significant milestone in its pioneering program with the country’s Ministry of Health, initiating more than 600 patients on lifesaving therapy for drug resistant TB at its two program sites at St. Peter's Specialized TB Hospital in Addis Ababa, and at Gondar University Hospital in the northern Ethiopian city of Gondar. To further the impact of its work, GHC plans to scale its programs to the north of Ethiopia in the Amhara region and the Southern Nations, Nationalities and People’s Region (SNNPR), following the community-based approach established in Cambodia. In addition, construction is also well underway at the Zahara Children’s Center in Sebeta, on the outskirts of Addis Ababa. Modeled on the Maddox Chivan Children’s Center in Phnom Penh, the Zahara Center will help meet the needs of the thousands of children infected with or affected by TB and HIV in the country, and will be the center to treat children with drug resistant TB in East Africa. |
|
| 2011 | Cambodia We have now treated almost 32,000 people for TB since our founding in 1994, growing and refining the community-based approaches we developed at the grassroots level. Our community-based TB program, Community Treatment Model has been adopted by the Cambodian Ministry of Health and has been expanded nationwide. We continue to deliver direct TB care to an area serving nearly two million people in three of Cambodia's poorest and war-affected provinces, Svay Rieng, Kompot, and Kandal. In 2011 CHC's AIDS programs delivered primary HIV care to 4,300 adults and 1,000 children in urban and rural Cambodia. Our rural AIDS program was the first to integrate TB and AIDS care in the country, providing a global model for the treatment of these diseases. In Phnom Penh, the pulmonary ward of the largest public hospital where CHC works, has been transformed into a center of excellence for TB and HIV care in part due to the CAMELIA clinical trial; a trial CHC's clinical network conducted that showed a 33% decrease in mortality from TB and HIV co-infection by changing the timing of AIDS drugs routinely used in Asia and Africa. At the Maddox Chivan Children's Center, 295 children received ongoing medical, nutritional, educational and social care in 2011. And 360 HIV-positive children received their HIV care at the Joseph P. Sullivan Outpatient Center of Excellence for TB and AIDS Care of Children at the Khmer-Soviet Friendship Hospital, Phnom Penh's largest public hospital where the social programs of the Maddox Center have been integrated. In addition, we have screened close to 2,000 Cambodian TB patients for drug-resistant TB and placed 200 on drug-resistant TB therapy. Our aim is to scale up access for universal care for drug-resistant TB nationwide, a global first. Our commitment to children with TB also expanded this year. We conducted a pediatric TB diagnostic study that screened more than 2,600 children to validate promising new diagnostic tools and to determine the burden of TB among very young children in rural Cambodia. Each year at least one million children develop TB and 500,000 die worldwide. Most of the deaths are due to challenges in diagnosing the disease. The CHC established the GeneXpert system, the first in Asia which can diagnose TB in two hours on pediatric samples, potentially saving up to 150,000 lives each year. Ethiopia At year end in a pioneering program with the country's Ministry of Health, 342 patients had begun therapy for drug-resistant TB at our two program sites at St. Peter's Hospital in Addis Ababa, and at Gondar University Hospital in the northern Ethiopian city of Gondar. Many of these patients are very young and have permanent lung and heart damage, having had to wait years for curative drugs to come to Ethiopia. They face the two years it takes for a cure of drug-resistant TB in our program, which has one of the best records of cure/completion and adherence to care in the world. It is being recognized as a model to scale up and provide access to drug-resistant TB care in Africa and other resource poor settings. A quarter of our patients are co-infected with HIV. In a significant milestone, we have broken ground on the Zahara Children's Center on the outskirts of Addis Ababa. The center will merge the lifesaving strategies developed at the Maddox Chivan Children's Center in Cambodia with the needs of the tens of thousands of children infected with or affected by TB and HIV in Ethiopia. There are approximately 135,000 children under the age of 14 living with HIV Ethiopia and approximately one million AIDS orphans. We expect the center to open in the spring of 2013. |
|
| 2010 | Cambodia CHC's community-based treatment model for TB, begun in 3 district hospitals in 1994 in Svay Rieng Province, has now been expanded countrywide to cover all 15 million Cambodians through the Cambodian National TB program; CHC is directly delivering TB care to three of Cambodia's provinces, Svay Rieng, Kompot and Kandal. With continued support from the Jolie-Pitt Foundation, CHC's Maddox Chivan Children's Center has served close to 1000 HIV-infected or -affected children with medical, nutritional, educational, social, and vocational programs. A major achievement of 2010 has been the completion of a counseling manual to help children of different ages to understand their HIV infection and the importance of taking drugs daily. Its translation into Khmer and Amharic are underway and we anticipate it will be used globally. With support of the Annenberg Foundation, CHC has expanded access to treatment for drug-resistant TB in Cambodia with the goal of universal access to drug-resistant TB care for all Cambodians, creating a model of community- and home-based care, in partnership with the National TB program. The CHC-led clinical trial (CAMELIA) supported by the U.S National Institutes of Health (NIH), and the French Agence Nationale Recherches sur le SIDA was concluded and its first results were presented at the International AIDS conference in July. The results show that initiating AIDS therapy 2 weeks after beginning TB drug therapy decreases mortality by 34%. These results, which will change global practice and save tens of thousands of lives, were recently cited by the NIH as one of the 2010 landmark discoveries for AIDS. CHC's Joseph P. Sullivan Outpatient Center of Excellence for TB and AIDS Care of Children at the Khmer-Soviet Friendship Hospital (KSFH), Phnom Penh's largest public hospital is providing care for more than 400 HIV-positive children, and enhancing services for all children at the hospital, with a particular focus on neonatal care in 2010. The CHC's program at the pulmonary ward at the Khmer-Soviet Friendship Hospital in Phnom Penh, which was once a dilapidated ward for destitute adult TB and AIDS patients, has been transformed by CHC into a teaching ward and the Cambodian Center of Excellence for AIDS and TB care and has provided care for over 1200 patients since 2006. CHC's community based provincial AIDS programs, the first to treat AIDS at the provincial level and to integrate TB and AIDS care in Cambodia, now provides treatment and follow-up for over 5,000 patients. CHC is working to prevent the suffering that TB causes to children and their families and is currently implementing one of the largest pediatric TB diagnostic studies in Svay Rieng, the first of its kind in South-East Asia. The study will help deliver TB care to children under 5 and provide knowledge to find better ways to diagnose TB in children. CHC is pioneering the new Gene Xpert technology to speed up diagnosis. Ethiopia After training in Cambodia, Ethiopian doctors together with Global Health Committee, began the first-ever treatment program for treatment for drug-resistant TB in Ethiopia in February 2009. Supported by the Jolie-Pitt Foundation, by January 2011, the program had initiated 171 patients on therapy. Most of the patients had been waiting for years for therapy and were extremely ill. Planning for National scale-up of this pioneering program with the Ethiopian Ministry of Health is underway. The drug-resistant TB program was expanded to the north of Ethiopia to Gondar in August 2010 in a collaboration between GHC, the Ethiopian Ministry of Health, and Gondar University Hospital. Based on the successes in Ethiopia, GHC/CHC presented a keynote talk "Working with National TB Programs Across Two Continents: Opportunities and Challenges" at the WHO's expert Consultation Meeting to Strengthen Engagement of Civil Society Organizations in the TB Area of Work of the WHO, in Geneva in Sept. 2010. Berlin (Germany) based Graft Lab architects design the Zahara Center for AIDS- and tuberculosis-affected children in the outskirts of Addis Ababa, modeled after the CHC's successful Maddox Chivan Children's Center in Cambodia. GHC/CHC's work was featured in the photo exhibition of James Nachtwey at 401 Projects in NY, NY and in his video on drug-resistant TB, ‘Struggle for Life'; was written up in the international journal Nature, as having developed a pioneering community-based approach to HIV and TB care and research, was featured on the Women's Conference website, and was the subject of two ABC news reports on Good Morning America and World News Tonight showing the impact of the work. |
|
| 2009 | Cambodia CHC's community-based treatment model for TB has been expanded countrywide to cover all 15 million Cambodians through the Cambodian National TB program. The CHC is directly supervising and delivering TB care in the three most populated Cambodian provinces. With support from the Annenberg Foundation, the CHC expanded access to treatment for drug-resistant TB to 144 patients, from 62 last year. Using our powerful model of community- and home-based care, we aim to provide universal access to drug-resistant TB care in partnership with the National TB program. GHC/CHC opens the Joseph P. Sullivan Outpatient Center of Excellence for TB and AIDS Care of Children at the Khmer-Soviet Friendship (KSF) Hospital, Phnom Penh's largest public hospital. Outpatient care is provided for more than 400 HIV-positive children, and an accompanying renovation of the pediatric ward has enhanced services for all children at the hospital. With continued support of the Jolie-Pitt Foundation, CHC's Maddox Chivan Children's Center serves more than 700 HIV-infected or -affected children with medical, nutritional, educational, social and vocational programs at the Maddox itself and at the Sullivan Center. CHC-led clinical trial (CAMELIA) of combined TB and AIDS treatment enters its final phase. CHC began a study of tuberculosis in children aimed at interrupting infection, funded by the AERAS TB Global Vaccine Initiative and the Gates Foundation. CHC researchers at Harvard Medical School and the Immune Disease Institute in Boston and at the Institut Pasteur du Cambodge in Phnom Penh, receiving key support from the Annenberg Foundation, the NIH, and the ANRS, continue their collaboration to develop new treatments for the "paradoxical reaction," a severe side effect that complicates HIV treatment in one-fifth of TB-infected patients. Ethiopia After training in Cambodia, Ethiopian doctors began the first-ever treatment program for drug-resistant TB in February 2009. The new program, which is supported by the Jolie-Pitt Foundation, is working with the Ministry of Health and the GHC. GHC/CHC obtains free medicines to treat drug-resistant TB in Ethiopia from Eli Lilly, the Chao Center of Purdue University, and Jacobus Pharmaceuticals. To date, 74 patients have received life-saving drug-resistant TB medicines and care under the new program. Plans for national scale up of the program are underway. Architects begin work on Zahara Center for AIDS- and tuberculosis-affected children in outskirts of Addis Ababa, modeled after CHC's successful Maddox Chivan Children's Center in Cambodia. |
|
| 2008 | Cambodian National TB program scales up CHC's community-based treatment model to cover the entire country. The CHC expands its operations outside Cambodia, to Southeast Asia and Africa. To reflect this international expansion, the organization takes on a new name, the Global Health Committee. GHC/CHC breaks ground on the Joseph P. Sullivan Outpatient Center of Excellence for TB and AIDS Care of Children at the Khmer-Soviet Friendship Hospital, Phnom Penh's largest public hospital. Renovation and modernization of the existing children's ward and addition of a new outpatient wing are all supported by a gift from Jeanne Sullivan in memory of her husband, a long-time CHC supporter and tireless advocate for refugees and human rights. In Phnom Penh, GHC/CHC takes charge of outpatient care for nearly 300 HIV-positive children from the Maryknoll Missionaries and from the departing Médecins Sans Frontières. GHC/CHC develops a new model for treating drug-resistant TB in hospitals and in the community. Working with the Cambodian government, the GHC/CHC obtains free medicines from the World Health Organization and UNITAID and sets a goal of universal access to drug-resistant TB treatment in Cambodia. GHC/CHC researchers at Harvard Medical School, the Immune Disease Institute in Boston and the Pasteur Institute of Phnom Penh begin an NIH-funded study in Cambodia to investigate the "paradoxical reaction", a severe immune side effect that complicates HIV treatment in one-fifth of TB-infected patients. GHC/CHC's TB and AIDS work featured in major photography exhibits in Paris, New York and Bangkok by award-winning Time Magazine photojournalist James Nachtwey, who is working to raise world awareness of drug-resistant tuberculosis and the link between TB and AIDS. CHC receives a two-year $500 thousand grant from the Annenberg Foundation for TB and AIDS treatment programs in Cambodia and research at the Immune Disease Institute in Boston. The grant recognizes the power of combining clinical care and discovery in the fight against TB and AIDS. GHC/CHC doctors train colleagues from Viet Nam and partner with them to initiate treatment of extensively drug resistant (XDR) TB with a donation of medicines from Eli Lilly and Co. GHC/CHC makes its first site visit to Swaziland, consulting with the national TB program to improve case detection and care for conventional and drug-resistant TB and TB/HIV coinfection using CHC Community Treatment Model. GHC/CHC receives $2 million gift from the Jolie-Pitt Foundation for work in Ethiopia. Planning starts for a center for AIDS- and tuberculosis-affected children in Addis Ababa, modeled after CHC's successful Maddox Chivan Children's Center in Cambodia. GHC/CHC conducts training in Ethiopia for physicians and nurses to begin drug-resistant TB treatment there, and Ethiopian medical workers travel to Cambodia for additional hands-on training from GHC/CHC staff. Recruitment in CAMELIA trial continues, nearing goal of 660 patients. |
|
| 2007 | James Nachtwey's photo exhibit at the United Nations, "A World Free of TB," spotlights the efforts of the CHC. To provide universal access to drugs for drug-resistant TB, CHC develops a countrywide treatment plan at the request of the National TB Program, and receives Green Light Status from the World Health Organization to obtain low-cost drugs for the program. CHC convenes the first Drug-resistant TB Working Group Conference to develop the Cambodian national guidelines for treatment and prevention of drug-resistant TB. The CAMELIA trial recruits its 382nd patient. |
|
| 2006 | CHC opens Maddox Chivan Children's Center (MCCC) in Phnom Penh, with the support of Angelina Jolie, providing a new model of integrated medical care, education, and social support to children infected or affected by AIDS. Marie-Pierre Fernandez leads this effort as its director. Cambodian National TB Program officially adopts CHC treatment model country-wide. First Cambodian patients begin CAMELIA trial. CHC is featured in three People Magazine issues sponsored by the Jolie-Pitt foundation, with photos by James Nachtwey. |
|
| 2005 | The CHC opens an AIDS treatment clinic at Kompong Trach District Hospital in Kompot Province, making it the most rural area to have access to AIDS treatment. Didier Laureillard leaves MSF France and becomes the first CHC medical coordinator, a position he will hold for two years, helping to launch the CAMELIA trial. CHC works with Japan International Cooperation Agency to expand TB treatment and Community Treatment Model to all of Svay Rieng province. Svay Rieng village bank microloan program, started by CHC in 1994, becomes an independent Cambodian Microfinance Institution dedicated to alleviating poverty. Sok Thim named a Hero of Global Health by TIME Magazine, which profiles him, Goldfeld and the CHC in its focus issue on global health. |
|
| 2004 | The NIH/CIPRA expands the planning grant to a five year, $2.5 million grant to build a clinical and research network for TB and AIDS and to support the CAMELIA trial. With support from US NIH and the Japanese embassy, CHC begins to renovate and upgrade the TB care facilities in the pulmonary ward of the largest hospital in Phnom Penh (KSFH, the Khmer-Soviet Friendship Hospital), which serves the poorest and sickest Cambodians dying from both diseases. With the support of the Sullivan Foundation and the American Foundation for AIDS Research TREAT Asia initiative, the CHC starts a pioneering at-home AIDS treatment program for AIDS patients built upon its TB treatment model. The program is based on the successful CHC TB model, using community health workers, patient supporter, education, treatment contracts, and food. It allows patients to receive care near their homes so they do not have to seek care in Phnom Penh where cut off from social supports they often end up homeless, sick and dying. CHC opens an AIDS clinic and inpatient ward at the Svay Rieng Provincial Hospital, the first rural Cambodian managed AIDS project. Thim and Goldfeld publish results of community-based TB treatment in JAMA. Their work ensconces the practice of combining microloans with food aid and Community Treatment Model in TB and global health care. |
|
| 2003 | As an outcome of the CIPRA planning process, the CHC develops a proposal to carry out the CAMbodian Early vs. Late Introduction of Antiretrovirals (CAMELIA) trial, which will establish the best timing of medication regimens for patients with both TB and AIDS. The study, the first of its kind, receives funding from the French ANRS and will be done in collaboration with the US NIH funded CIPRA. To raise global awareness of AIDS and TB, Goldfeld initiates a project with photojournalist James Nachtwey to document the twin epidemics in Cambodia. His photoessay, TB in Cambodia, is part of a portfolio that garners the Magazine Photographer of the Year award from the National Press Photographers Association. With support from the Jeanne and Joseph Sullivan Foundation CHC is able to buy AIDS drugs for 100 patients for one year. Dr Didier Laureillard, the medical coordinator of MSF France's pioneering AIDS treatment program in Phnom Penh serves as an advisor to CHC. |
|
| 2002 | CHC receives planning grant from the United States National Institutes of Health under the Comprehensive International Program of Research on AIDS (CIPRA) to establish a TB and AIDS clinical and research network throughout Cambodia. This leads to an extensive planning process engaging the French Agence Nationale Recherches sur le Sida and Cambodian governmental health agencies to achieve this goal. Goldfeld and Sok Thim return to Afg hanistan and Pakistan refugee camps (hear Chicago Public Radio interview). ARC subsequently establishes the largest health care program for Afghan refugees in the Quetta area and begins AIDS prevention activities in the camps. Goldfeld writes and speaks about the devastating TB problem in Afghanistan and its heavy toll on women. |
|
| 2001 | CHC begins treating hard-to-cure cases of drug-resistant TB in Svay Rieng. The program treats people in their homes using community health workers, patient supporters and individually tailored regimens of drugs (Community Treatment Model). Goldfeld and Sok Thim spread the CHC model by traveling to Pakistan and Afghanistan with the American Refugee Committee to establish AIDS and TB treatment programs in refugee camps there. CHC-USA incorporated as a tax-exempt 501(3)b charity. |
|
| 2000 | Sok Thim and Goldfeld publish Curing Tuberculosis: A Manual for Developing Communities. Goldfeld and team discover a unique immune reaction in patients that helps the TB bacterium evade host defenses. It is later found that this mechanism is a general mechanism by which the host immune system is regulated in many infectious diseases. Goldfeld begins a long-term research project in the Peruvian highlands around Cusco. The study of Quechua people will help to understand the genetic causes for differences in the immune response to TB. |
|
| 1999 | Community Treatment Model program begins: Mobile health teams fan out from district hospitals to deliver TB medications to villagers in remote locations daily. Health workers use village bank networks to seek out TB infected villagers for treatment. |
|
| 1998 | Goldfeld's research with Cambodian patients uncovers the first susceptibility gene for TB, which helps explain why some people become sick with the infection, and others do not (hear a Boston Public Radio interview of Goldfeld describing the discovery and its follow up from 2006). |
|
| 1997 | With additional private funding, the CHC expands its TB treatment program to Kompot, another poor and war-affected province in southern Cambodia, that had been a Khmer Rouge stronghold up until a few months before. CHC begins HIV/AIDS prevention programs in Svay Rieng and Kompot, providing education about the disease to high-risk groups and teens using peer group counseling and its extensive community and village bank networks. |
|
| 1995 | Research program on TB begins, in partnership with Goldfeld's laboratory at Harvard Medical School and later at the IDI Institute for Biomedical Research in Boston, Massachusetts. Goldfeld sees the opportunity to collaborate with the Cambodian patients and health workers to make significant progress into understanding the immune response to TB, and to develop new therapies linking delivery of care with basic scientific discovery. |
|
| 1994 | The CHC is officially founded in Svay Rieng, Cambodia, by Sok Thim, Goldfeld and Brian Heidel, Cambodian Country Director for the ARC, with a mission to deliver tuberculosis treatment to rural residents. In founding CHC they overcome international skepticism that community based care for TB could be successful in Cambodia or elsewhere. With a private donations, a TB program is started in the spring of 1994 using some approaches from the successful ARC camp program, but modified to meet the needs of impoverished and isolated residents in one of Cambodia's poorest provinces. Working out of three district hospitals in collaboration with the National TB Program, CHC rapidly expands to include free medicine, food assistance (in partnership with the World Food Program), patient supporters and community health workers and a novel village bank/microloan program. Beginning with a cadre of health workers trained by ARC in the border camps, CHC focused on the development of community health workers and joined forces early on with Ministry of Health doctors and the Cambodian National TB program providing training and support to them. This alliance ensures that the CHC's work will be sustainable and not just a boutique health delivery program. In partnership with OxFAM America and later with Catholic Relief Services, CHC initiates the first microfinance program linked to a TB treatment program, based on the Grameen bank model. The CHC Village Bank program goes on to make approximately 20,000 loans, and uses its profits to train village health workers. TB patients whose families participate in the village bank program have close to 100% adherence with TB medicines and similar cure rates. The dozens of village health workers trained with interest from the loans turn out to be key players in spreading information about the new epidemic of AIDS that is gripping Cambodia. CHC continues to refine its system of training community health workers, enlisting relatives as patient supporters and drafting treatment contracts, which eventually becomes the standard for outpatient TB treatment throughout Cambodia. The technique is also used as the base for other models of TB and AIDS care globally. Goldfeld testifies before the United States Congressional Hunger Caucus on Tuberculosis and Poverty in Cambodia. |
|
| 1993 | Sok Thim travels to Boston to finish the TB treatment manual with Goldfeld, and together they make plans to start a TB program in Cambodia. The first case of AIDS is diagnosed in Cambodia. |
|
| 1992 |
|
|
| 1989-90 | Sok Thim takes over management of the ARC TB treatment program from Maat and eventually becomes the head of all camps for the United Nations Border Relief Organization, an international effort to aid Cambodians and others affected by years of warfare along the Thai-Cambodian border. Goldfeld, who has completed her training in internal medicine and infectious disease, makes her first visit inside war-ravaged Cambodia, which is still under an international trade and aid embargo. She works briefly as a medical advisor to the Mennonite Central Committee there, then assumes the position of medical coordinator for ARC at Site II where she meets Sok Thim. Goldfeld and Thim begin to compile the case histories of all the TB patients treated in the camps, and pool their expertise to write a manual to treating the disease among refugees in war zones and in developing countries. At Site II, Goldfeld also initiates the land mine injury prevention program, in response to her experience caring for impoverished refugees who were injured by landmines while scavenging for food outside the camps. She makes the first call for a ban on landmines in 1991, in Congressional testimony before the US House Foreign Affairs Committee. Goldfeld becomes a leading voice in the fight against land mines, publishing articles and photos in outlets including the New York Times, Washington Post, Boston Globe and The Nation, making the link between poverty and victimization by landmines. She founds the US Campaign to Ban Landmines with Holly Myers in 1994, and serves as an advisor to the International Campaign to Ban Landmines, which goes on to win the Nobel Peace Prize in 1997. |
|
| 1988 | Goldfeld continues her work on behalf of refugees, and is the lead author on the first peer- reviewed scientific article on the medical effects of torture, which appears in JAMA (the Journal of the American Medical Association), which for the first time shows that rape is a common form of torture that women undergo in situations of war. |
|
| 1984 | Miles and Maat publish their landmark article on Community Treatment Model in Nong Samet. Their results show nearly 100 percent adherence to medicine and many cures, despite the difficult conditions in the camps. Sok Thim moves from nursing to ARC's medic training course and eventually becomes Maat's assistant. He becomes head of the TB treatment program in Site II, a new camp built after Nong Samet comes under attack by Vietnam-based Cambodian troops on Christmas Day. During the immediate evacuation of refugees all TB patients regrouped at the evacuation site and none missed a dose of TB medicines. |
|
| 1983 | Refugee Sok Thim arrives in Nong Samet with his family. He begins nursing training in the ARC school. ARC volunteer Anne Goldfeld, MD, a resident training in Internal Medicine at Massachusetts General Hospital (MGH) and Harvard Medical School, arrives in Nong Samet for the first time. |
|
| 1981 | Steven Miles, MD and Bob Maat of ARC argue that TB can and must be treated . Working from thatch-roof buildings with no electricity, they start a program in the Nong Samet refugee camp. Using a new antibiotic regimen that shortens the treatment time from one year to six months, they enlist family members as patient supporters and provide food along with the medicines. Their program marks the first use of the new Community Treatment Model in an active war zone. |
|
| 1980 | ARC recognizes tuberculosis as a leading health problem in camps. While curable, the disease is notoriously hard to treat, requiring a year-long regimen of multiple drugs. Because drug resistance threatens to emerge whenever treatment is interrupted, the international health community opposes a TB treatment program in the camps, fearing there is no way for dispossessed refugees to complete the arduous treatment. |
|
| 1979 | Vietnamese troops occupy war-torn Cambodia, a country that has been in the grips of the genocidal Khmer Rouge regime, which has already killed 1 million Cambodians. When the regime falls, another 1 million starving people flee west to refugee camps on the Thai border. American Refugee Committee is founded in Minneapolis and Chicago to aid Indochina Refugees, and begins a program of health worker training in Cambodian camps. |


